What is Hepatorenal Syndrome?
Hepatorenal syndrome is a violation of various functions of the liver or kidneys in the event of a pathological process in one of these organs, as well as their simultaneous damage when exposed to endogenous and exogenous factors harmful to the body.
According to A. Ya. Pytelya (1962), hepatorenal syndrome develops after surgery on the biliary tract in 18% of patients. In persons suffering from various liver diseases, kidney damage is established I. Ye. Tareeva et al. (1983) in 10-20% of cases.
Causes of Hepatorenal Syndrome
The causes of liver and kidney damage are diverse. Most often develops hepatorenal syndrome in occupational intoxications and acute poisoning, after cardiac surgery with cardiopulmonary bypass and biliary tract, acute pancreatitis, viral hepatitis, sepsis, infections, burns, hemolytic reactions, medicinal lesions, circulatory disorders, etc.
When considering hepatorenal syndrome, the leading place is occupied by the question of the state of the kidneys in liver diseases, of which acute and chronic hepatitis, liver cirrhosis, and diseases of the biliary tract are of the greatest importance.
Pathogenesis during Hepatorenal Syndrome
The pathogenesis of kidney damage in liver diseases is complex and not well understood. According to most researchers, there are several major pathogenetic mechanisms that can lead to pathological changes in the kidneys in liver diseases. These are hemodynamic disturbances and direct effects on the kidneys of various metabolites, antibodies, immune complexes, etc. Some authors (A. F. Bluger et al., 1975; I. B. Tareeva et al., 1983) assign a certain role to bacterial endotoxins, especially Gram-negative lipopolysaccharide, intestinal microbes that cause renal vasoconstriction and create favorable conditions for intravascular coagulation.
In injuries and surgeries on the liver and biliary tract, the occurrence of hepatorenal syndrome is also not completely understood. A number of reasons that negatively affect the renal blood flow are assumed: jaundice duration, severe hypotension, irritation during nerve receptor surgery (hepatorenal reflex), massive absorption of tissue breakdown products in trauma and operations, and previous diseases of the liver and biliary tract.
Regarding the state of the liver function in primary kidney lesions, the studies performed are few. However, they indicate the possibility of secondary changes in the liver when exposed to elevated concentrations in the blood of non-neutralized decay products of the body’s tissues, including the kidneys, especially during the inflammatory process in them, as well as microbial metabolic products. The most frequent abnormal liver functions are found in patients with chronic pyelonephritis, in which the above factors can apparently affect the liver simultaneously.
With liver damage on the background of primary kidney disease, according to A. F. Blugera et al. (1975), morphological changes in the hepatic tissue are different and depend on the severity and duration of the pathological process in the kidneys: from hepatocyte dystrophy and moderate mesenchyme reaction to degenerative-inflammatory processes that lead to a gross restructuring of its structure.
Symptoms of Hepatorenal Syndrome
Detailed classifications of hepatorenal syndrome depending on the etiological factor and the sequence of development of changes in the liver and kidneys are recommended by A. Ya. Pytel (1983), A. F. Blyugher et al. (1975), B.N. Shulutko (1976) and others.
In practice, there are two clinical variants of hepatorenal syndrome. At the first stage, there are no subjective and objective signs of this syndrome, only an increase in the blood of liver enzymes, hypergammaglobulinemia, moderately increased ESR, and leukocytosis are detected; in urine sediment – in a small amount of protein, red blood cells, white blood cells, hyaline cylinders. However, the main functions of the liver and kidneys are not affected. In the second embodiment, there is a failure of the main functions of the liver and kidneys of varying severity. Asthenia, fatigue, headache, abdominal and lower back pain, dyspepsia, dysuric phenomena, edema, hemorrhagic diathesis are noted. Distinctive violations of the bilirubin, albumin-producing and cholesterol-esterifying functions of the liver are found; in the blood, the level of prothrombin is reduced and the level of residual nitrogen, urea, creatinine is increased. On the part of the kidneys, oliguria, proteinuria, erythrocyturia, leukocyturia, decreased concentration function, glomerular filtration, and tubular secretion of varying severity are found.
Practice shows that carrying out complex treatment aimed at eliminating harmful factors and restoring impaired liver and kidney functions is often successful.
Diagnosis of Hepatorenal Syndrome
The above variants of the clinical course of hepatorenal syndrome are found in the kidneys or in the liver with diseases of one of these organs or with their simultaneous damage as a result of exposure to various harmful factors. If these reasons are eliminated, but the complete reverse development of the pathological process in the liver or kidneys did not occur, in these cases the hepatorenal syndrome should be differentiated from such diseases of these organs as hepatitis, cholecystitis, cholangitis, glomerulonephritis, pyelonephritis, etc.
Treatment of Hepatorenal Syndrome
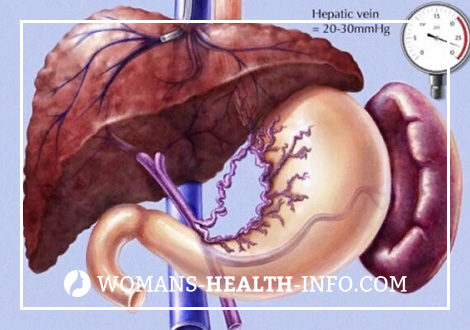
Simultaneous damage to the liver and kidneys presents certain difficulties in treatment and requires consideration of many factors. The similarity of the pathogenesis of a number of diseases of the liver and kidneys, metabolic disorders of proteins, fats and mainly electrolytes, tissue hypoxia is determined by the uniformity of some therapeutic effects. However, there are significant differences that require selective therapy. Observations in the clinic show that the complete reverse development of the hepatorenal syndrome is possible with the restoration of impaired liver or kidney functions, the elimination of harmful factors. Therefore, I. Ye. Tareeva et al. (1983) believe that treatment for hepatorenal syndrome should be complex and aimed primarily at reducing hepatic cell insufficiency and reducing portal hypertension, both surgically and conservatively.
Eliminating or reducing the negative effects of etiological moments on the body also plays a significant role in the successful treatment of the hepatorenal syndrome.
Bed rest is necessary both for liver and kidney diseases, but it is more stringent for kidney diseases. Here it is necessary to bear in mind the negative impact of active movements on the renal circulation. Sufferers of hepatorenal syndrome should observe strict bed rest (with extrarenal symptoms for 4-6 weeks, with isolated urinary syndrome for 3-4 weeks).
If in case of hepatorenal syndrome occurring without renal and hepatic insufficiency, the amount of protein administered is not substantially limited, then in the presence of signs of hepatic and renal insufficiency, it is often necessary to reduce its amount. However, in severe hypoalbuminemia, parenteral administration of albumin should be prescribed. The amount of injected fats and carbohydrates is not limited and is determined by the necessary energy intake.
In patients with hepatorenal syndrome without portal hypertension and extrarenal manifestations, the amount of sodium chloride administered is not limited. However, during the formation of portal hypertension, even in the absence of fluid in the abdominal cavity, in the presence of extrarenal signs (edema, high blood pressure), it is necessary to limit the administration of sodium chloride, often up to 2-3 g per day, i.e. in products. To improve the taste of food you can add potassium chloride (in the absence of hyperkalemia). With severe hepatoreal syndrome, accompanied by diarrhea, vomiting, a large amount of sodium chloride is lost, so it must be introduced additionally in the form of isotonic or hypertonic solution.
Complications of hepatorenal syndrome are often anemia. Therefore, foods rich in iron and cobalt (egg yolk, green peas, buckwheat, beets, lingonberries, strawberries, etc.) should be recommended as food for patients.
Drug treatment of hepatorenal syndrome presents certain difficulties. To normalize the impaired functions of the liver and kidneys, vitamin therapy is indicated, which increases the effectiveness of the therapeutic effect of many drugs. It is advisable to introduce vitamins C – 500 mg, BI (thiamine) – 50, B2 (riboflavin) – up to 50, PP (nicotinic acid) – up to 300 mg in fractional doses, B6 – up to 100-200 mg, B12 – up to 200 mg per day .
Glucocorticosteroid hormones are most effective in treating a number of liver and kidney diseases. Indications for the appointment of hormone therapy are protracted forms of acute hepatitis, exacerbation of chronic, mainly biliary form of cirrhosis, as well as acute development of liver failure, complicated by pathological changes in the kidneys. Corticosteroids can be used both independently and in combination with 4-aminoquinoline preparations or cytotoxic drugs with a reduced dose of hormones. Since the inactivation of hormones is reduced in case of diffuse lesions of the liver, it is sufficient to prescribe 15–20 mg, a maximum of 30–40 mg of prednisolone per day. The dose of hormones should be adjusted according to the severity of the process and the patient’s body weight. The course of treatment with maximum doses of hormones is at least 3 weeks, then the dose is gradually reduced at the rate of 2.5 mg in 2-3 days.
High blood pressure, lipid disorders, diabetes mellitus, peptic ulcer disease and other conditions are contraindicated corticosteroids, in such cases, as well as the ineffectiveness of corticosteroid therapy is expedient to appoint immunosuppressive agents, cytotoxic agents and drugs 4 aminohinolinovogo series: azathioprine, mercaptopurine, cyclophosphamide, leukeran (chlorbutin), delagil, plaquenil. These drugs can be prescribed to patients alone or in combination with small doses of prednisone (in the absence of contraindications) for 6-8 weeks, followed by a switch to maintenance doses (1/3 – 1/4 of the treatment dose). Indomethacin has a slight immunosuppressive effect. However, nonsteroidal drugs (metindol, Brufen), as well as immunosuppressants and cytostatics, are contraindicated in liver cirrhosis, since they can contribute to the development of hepatorenal syndrome and in large doses are hepatotoxic. The mentioned hormonal and immunodepressive therapy should be carried out under the guise of antibiotics, especially in the presence of foci of infection.
In addition to basic therapy, patients with hepatorenal syndrome, developed on the background of chronic hepatitis, are shown drugs that improve the exchange of liver cells. To prevent the progression of hepatocellular insufficiency, disorders on the part of protein and electrolyte metabolism should be eliminated: albuminemia, hypokalemia, ammonium. This is achieved by intravenous administration of albumin, potassium preparations (panangin, potassium chloride, etc.), sterilization of the large intestine with antibiotics (monomitsin – 0.25 g 4-6 times a day inside; polymyxin B – 0.1 g 4 times a day inside ).
When signs of hepatic precoma appear, prednisone is shown (200-300 mg or more per day), oxygen therapy, if possible, in a pressure chamber.
In the event of esophageal-gastric bleeding, fresh blood transfusion directly from the donor is recommended, the appointment of aminocaproic acid, Vicasol, calcium chloride; apply gastric hypothermia, balloon tamponade, make emergency ligation of varicose veins. In some cases, with sufficient preservation of liver function shows the imposition of portocaval anastomosis.
As for the kidneys, symptomatic treatment for hepatorenal syndrome should be aimed at increasing diuresis, reducing azotemia, compensating for water and electrolyte disorders. It is advisable for such patients to use perirenal blockade, glucosonovocaine mixture, according to indications – b-adrenoblockers, aminophylline, saluretics, heparin, polyglucin, reopolyglucin, hemodez, potassium preparations.
Prevention of Hepatorenal Syndrome
It is possible to prevent the development of hepatorenal syndrome by timely detection and treatment of the pathological process that has arisen in the liver, kidneys and other organs and systems, as well as by preventing various exogenous harmful factors from affecting the body.
Dispensary observation of patients with hepatorenal syndrome after the main course of treatment in a hospital should be carried out by the relevant polyclinic specialists, and in their absence, the local physicians in the main nosological form of the disease that caused the hepatorenal syndrome, using the dynamic monitoring schemes approved by the health authorities.